Hi everyone,
Scientific research based on combating drug resistance is becoming increasingly important– a very current topic due to the rise of drug-resistant superbugs. However, contrary to what is widely discussed in the news and other public domains, drug resistance isn’t just limited to dangerous infections such as MRSA. It can also actually cause huge problems in the treatment of diseases such as cancer.
Building on decades worth of research into intensive disease modelling and drug therapies, a new study in PNAS provides a solution to the problem of therapeutic resistance. This is through adaptive therapy, which improves the way that drugs are used in treatment in such a way that the risk of therapeutic resistance is dramatically reduced. After learning more about it, I can honestly say that the emerging of adaptive therapy treatments needs to be discussed more as a viable, effective approach to managing and treating several terminal illnesses.
The basis of adaptive therapy is straightforward and built upon the traditional treatment of diseases. Most of the time when we get infected with a pathogenic disease such as cancer, if the drug used in the treatment doesn’t work, then the likelihood is that the cancer cells will probably have become resistant. Typically, when scientists encounter this, the solution is to develop a new drug.
Although this certainly solves the short-term problem of treating the disease, it doesn’t actually solve the problem of therapeutic resistance.
Unfortunately, due to the aggressive nature of many of these diseases, the problem with many terminal illness drug treatments is that they use a very high dose. When you push infectious diseases too hard with the highest tolerable drug dose, you inevitably force them to evolve drug resistance.
In order to avoid this happening, this new study suggests a different but effective therapeutic approach to maintain the disease, rather than eradicate it. An example of this could be through the treatment of cancer. Instead of trying to eradicate the cancer cells and running the potential of drug resistance evolving within the cancer cells, treatment would involve maintaining a small population of disease cells in the patient’s body that are low enough to ensure the patient does not feel ill. Providing the disease develops slowly, this strategy could be used for an extended period of time.
I had the pleasure of speaking to Newcastle University’s Dr Sergey Melnikov, lead scientist on this research which was largely based at Yale University. Sergey explained that in a prostate cancer model, during treatment instead of using the maximum tolerable dose, drug treatment should only be used in a quantity and duration that is enough to reduce the PSA (prostate-specific antigen) levels (PSA levels rise when the prostate is cancerous). Once the levels have dropped sufficiently, there would be a break without drug treatment, known as the ‘off-stage’. When the PSA levels begin to rise again, then the drug will be used again for a short period until the PSA levels reduce, followed again, by a break. This would be a continuous cycle.

The rationale for this approach is that during drug treatment, there will be a population of cancer cells that will become resistant to the drug (due to random mutations in the cell DNA). However, in the absence of the drug, these cells will become sick, because they have become dependent on that drug. They will, therefore, be outcompeted by healthier cells, until only non-resistant cells remain, and the drug-resistant cancer cells have been eradicated. This is purely thanks to natural selection due to drug-resistant mutations now being disadvantageous to the cells.
However, there is a natural problem with this therapeutic approach as cancer cells do not grow slower when using this treatment, so competition between cells is high. There are instances where this could work well, especially if the cell cycle is tightly controlled through therapeutic interventions, but obviously, this is riskier in cases of illnesses such as metastatic cancer (cancer that spreads to other organs).
Sergey explained that his work has therefore been based on looking at how to accelerate the natural evolutionary competition between resistant and non-resistant cells. By using E. coli as a model, the study demonstrated a way to increase resistance and shorten the drug-free phases of adaptive therapy, reducing the possibility of metastasis. The approach will also lead to increased elimination of drug-resistant cancer cells.
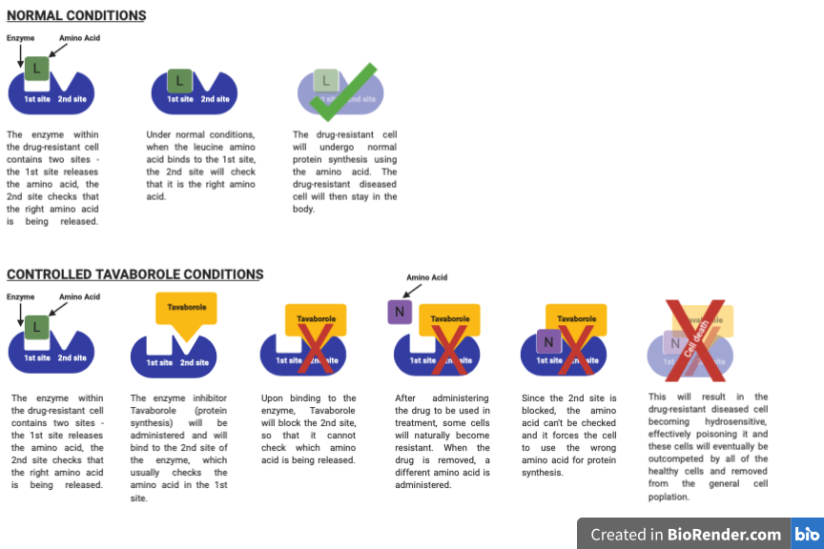
The experimental model involved a collaborative group of engineers who developed a system of small 3D printed bioreactors (growth chambers), where E. coli could be grown and the growth rate of cancer cells in response to drugs could be monitored. The group grew drug-resistant E. coli in the presence of a protein synthesis inhibitor; Tavaborole. Resistance to this inhibitor results from mutations in a gene that codes for a leucine amino-acid enzyme. This drug was targeted in this study because it is highly accurate for selecting leucine.
Now, there are two catalytic sites on the enzyme – the first site sends out the amino acid, and the second proofreads the process, preventing mistakes. The E. coli cells are treated with the Tavaborole which inactivates the second site. Treatment with the disease drug will then result in naturally occurring drug-resistance, and when the drug is removed during the ‘off’ cycle of the adaptive therapy, the addition of an amino acid that is similar to leucine will force the cell to use the amino acid instead of leucine for protein synthesis. As the proofreading section of the enzyme is blocked, this will not be picked up and the resistant E. coli cells then become hydrosensitive and in a selective way, it poisons them, removing them from the cell population and only leaving drug-sensitive cells.
By mixing drug-sensitive and drug-resistant E. coli at a 1:1 ratio and using genetic labelling via coloured red and green protein expression, the ratio of the E. coli cells can be monitored over time and eventually, only drug-sensitive cells will remain. This sort of technique would accelerate adaptive therapies, reduce the drug-free stages of treatment, so the fear of metastasis would be reduced.
Some of the ideas the research group had focused around are that there are many drugs on the market, some being natural and others synthetic. If a drug has multiple targets, then the evolution of drug resistance is unpredictable. Therefore, synthetic drugs with a single target would be best for therapeutic use. It is more difficult to predict non-synthetic resistance, as there are many ways that resistant evolution could co-occur. As Sergey explained, it’s all about predictable drug resistance.
This study demonstrates that it is possible to create an approach to combating drug resistance through adaptive therapy. There are thousands of drugs out there, but optimal use of these is just starting to be discovered. A study like Sergey’s shows that the principles of Darwin’s natural selection (survival of the fittest) could be used during disease treatment to prolong the effectiveness of drugs which could increase the time the disease goes into remission, and prolong life.
The biggest problem from here would probably be changing the public perception of cancer treatments. The status quo is very much an all or nothing approach, with many people just accepting that they will receive high doses of chemotherapeutic drugs. This new adaptive therapy approach is undoubtedly hugely advantageous to the patient but persuading them that it is ok to have periods where treatment is completely stopped may be a hard pill to swallow. Nevertheless, with increased research and clinician’s approval, I am sure that this is a revolutionary therapy that people should expect to see in clinics for years to come.
You can find Sergey’s research groups’ paper HERE, the preprint paper HERE, and you can find his contact details either on the paper, Newcastle University website HERE or the Melnikov Lab website HERE. His research is fascinating and I’d definitely encourage you to read more.
https://doi.org/10.1073/pnas.2003132117
https://doi.org/10.1073/pnas.2003132117
Until next time,
M x


Very interesting blog post.
LikeLiked by 1 person
Thank you very much for this wonderful post, Maria! Indeed, we witnessed something similar in agriculture where, in late 1970s, pesticide resistance caused a near-collapse of the cotton industry forcing scientists to develop the Integrated Pesticide Management philosophy – minimal application of pesticides as opposed to the nuclear blast doses pesticides – deliberate choice to manage pests and maintain them at acceptable levels rather than trying to eradicate them – these were new mottoes of that industry. And it boggles my mind that it took almost half a century to become equally serious about human health as we are serious about fruits and veggies…
LikeLike
Interesting blog-post. There is a strong counter argument to adaptive therapy. If you consider empirical evidence that tumour size is a time-dependent covariate for patient survival, you will find theoretically that adaptive therapy is worse than contonuous therapy, see here: https://www.biorxiv.org/content/10.1101/2020.06.23.167056v1.full
LikeLike